The varicella-zoster virus (VZV), a member of the herpesvirus family, is responsible for a range of medical conditions. Primarily known for causing chickenpox and herpes zoster (shingles), the virus can also lead to serious complications in vulnerable populations. Below is a detailed breakdown of VZV-related diseases and essential information about their presentation, risks, and management.
Chickenpox: Primary VZV Infection
Chickenpox is an acute, highly contagious illness caused by initial VZV exposure, most commonly affecting children. The disease manifests with a generalized rash progressing from macules to papules, vesicles, and crusts, accompanied by fever, fatigue, and itching. Transmitted via respiratory droplets or direct contact, the incubation period spans 10 to 21 days. While most healthy individuals recover without intervention, immunocompromised patients face risks of severe complications, including viral pneumonia, encephalitis, or secondary bacterial infections. Timely supportive care—such as antiviral therapy for high-risk cases—can mitigate severity.
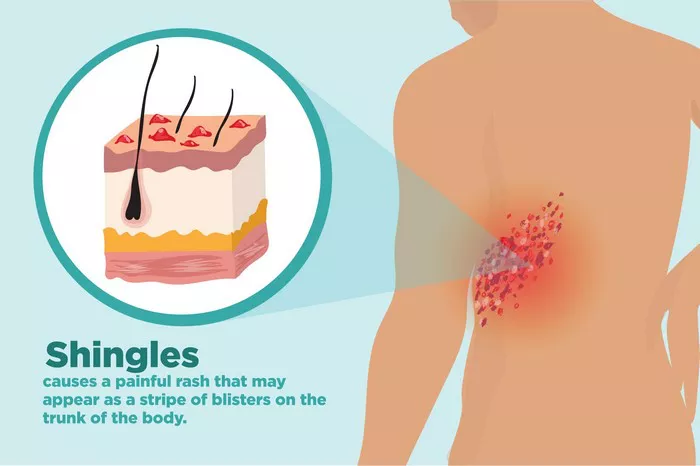
Herpes Zoster (Shingles): Reactivated VZV Infection
Herpes zoster occurs when the dormant virus reactivates in sensory nerve ganglia, typically in older adults or those with weakened immunity (e.g., due to age, chronic illness, or immunosuppressive therapy). Characterized by painful, unilateral clusters of vesicles along a dermatome (often thoracic, lumbar, or trigeminal regions), the condition is preceded by prodromal symptoms like tingling or burning. Acute pain lasts 2–4 weeks, and early antiviral treatment (within 72 hours of rash onset) reduces lesion duration and postherpetic neuralgia (PHN) risk.
Postherpetic Neuralgia (PHN): A Debilitating Complication
PHN affects 10–30% of shingles patients, defined by persistent neuropathic pain lasting months or years after the rash resolves. Risk factors include advanced age, severe acute rash, and intense initial pain. Symptoms range from burning, shooting, or stabbing sensations to heightened skin sensitivity. Treatment strategies include nerve block procedures, calcium channel modulators (e.g., gabapentin), tricyclic antidepressants, and topical therapies. Early intervention is critical to improve quality of life.
Herpes Zoster Ophthalmicus: Ocular Complications
Involvement of the ophthalmic branch of the trigeminal nerve (V1) leads to herpes zoster ophthalmicus, a serious condition requiring urgent ophthalmologic evaluation. Symptoms include eyelid edema, conjunctival injection, keratitis, iridocyclitis, and vision loss. Untreated cases may progress to corneal ulcers, scarring, or even blindness. Management combines systemic antiviral agents (e.g., acyclovir, valacyclovir) with topical corticosteroids to reduce inflammation and preserve ocular function.Disseminated Herpes Zoster: Systemic Spread in Immunocompromised Hosts
In individuals with profound immunosuppression (e.g., HIV/AIDS, cancer, or transplant patients), VZV can disseminate hematogenously, causing multi-organ involvement. Beyond widespread skin lesions, complications may include pneumonitis, hepatitis, encephalitis, or gastrointestinal involvement. This form carries a 5–15% mortality rate, necessitating aggressive treatment with intravenous antiviral therapy (e.g., acyclovir) and supportive care, such as immunoglobulin therapy in select cases.
Prevention and Management Strategies
Vaccination: The most effective preventive measure. Routine varicella vaccination is recommended for children ≥1 year, while the herpes zoster vaccine is advised for adults ≥50 years to reduce shingles risk and severity.
Symptomatic Care: During illness, maintain skin hygiene, avoid scratching (to prevent secondary infection), and wear loose cotton clothing. A nutrient-rich, vitamin-dense diet and rest support recovery.
Emergency Warning Signs: Seek immediate medical attention for severe symptoms, including persistent high fever, respiratory distress, altered mental status, or vision changes, which may indicate life-threatening complications.
Conclusion
The varicella-zoster virus presents a spectrum of diseases, from the self-limiting chickenpox to the potentially devastating complications of shingles. Understanding risk factors, recognizing early signs of severe illness, and prioritizing vaccination are key to public health management. Healthcare providers emphasize proactive care for high-risk individuals and timely intervention to mitigate long-term morbidity.
Related Topics: