Tinea, commonly known as ringworm, is a persistent and often recurring fungal infection affecting the skin, hair, and nails. Despite effective treatments available, many individuals find themselves battling repeated episodes of this frustrating condition. Understanding the reasons behind tinea’s recurrence is essential for both prevention and management. This article delves into the various factors that contribute to the persistence of tinea infections and offers insights into effective strategies for minimizing the risk of recurrence.
Understanding Tinea Infections
Tinea infections are caused by dermatophytes, a group of fungi that thrive on keratin, a protein found in the outer layer of skin, hair, and nails. These infections are classified based on their location on the body:
- Tinea Corporis: Affects the body.
- Tinea Pedis: Also known as athlete’s foot, affects the feet.
- Tinea Capitis: Affects the scalp.
- Tinea Cruris: Also known as jock itch, affects the groin area.
- Tinea Unguium: Affects the nails, also called onychomycosis.
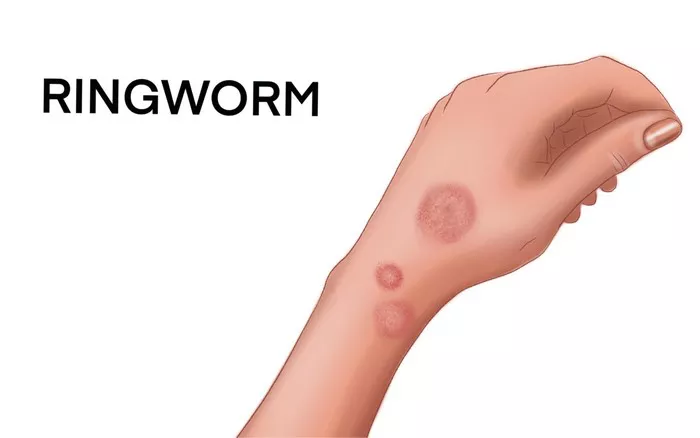
The characteristic symptoms of tinea include red, scaly, and often itchy patches that can spread and form ring-like shapes. Despite the name “ringworm,” no worms are involved in this infection.
Factors Contributing to Recurrence
1. Incomplete Treatment
One of the primary reasons for tinea’s recurrence is incomplete or inadequate treatment. Dermatophyte infections require a full course of antifungal medication to ensure complete eradication of the fungi. Stopping treatment too soon, even if symptoms appear to resolve, can leave behind resilient fungal spores that can cause a relapse.
2. Reinfection from the Environment
Tinea fungi are highly contagious and can be easily transmitted through direct contact with infected individuals, animals, or contaminated surfaces. Common sources of reinfection include:
- Shared personal items: Towels, clothing, hairbrushes, and bedding can harbor fungal spores.
- Public spaces: Locker rooms, swimming pools, and communal showers are hotbeds for fungal contamination.
- Pets: Animals, particularly cats and dogs, can carry dermatophytes and pass them on to humans.
3. Underlying Health Conditions
Certain health conditions can predispose individuals to recurrent tinea infections. These include:
- Immunosuppression: Conditions like HIV/AIDS, diabetes, and the use of immunosuppressive medications can weaken the immune system, making it harder to fight off infections.
- Skin conditions: Eczema, psoriasis, and other chronic skin conditions can compromise the skin barrier, providing an entry point for fungi.
SEE ALSO: Does Hand Sanitizer Kill Ringworm Fungus?
4. Personal Habits and Hygiene
Poor personal hygiene and habits can contribute to the persistence of tinea. These include:
- Inadequate drying: Fungi thrive in warm, moist environments. Not thoroughly drying the skin after bathing or exercising can create ideal conditions for fungal growth.
- Wearing tight or non-breathable clothing: Tight clothing, especially made from synthetic materials, can trap moisture and heat, promoting fungal proliferation.
- Infrequent changing of clothing and footwear: Wearing the same clothes or shoes for extended periods without washing or airing them out can increase the risk of reinfection.
5. Genetic Susceptibility
There is evidence to suggest that genetic factors can influence an individual’s susceptibility to dermatophyte infections. Some people may have a genetic predisposition that affects their skin’s ability to defend against fungal invaders.
Prevention Strategies
Preventing recurrent tinea infections involves a combination of effective treatment and lifestyle modifications. Here are some strategies to minimize the risk:
1. Complete the Full Course of Treatment
It’s crucial to follow the prescribed treatment regimen to completion, even if symptoms improve before the medication is finished. This ensures that all fungal spores are eradicated and reduces the likelihood of recurrence.
2. Maintain Good Hygiene
Adopting good hygiene practices is essential in preventing tinea reinfection:
- Regular bathing: Cleanse the skin daily and ensure thorough drying, especially in areas prone to moisture buildup.
- Avoid sharing personal items: Use separate towels, clothing, and grooming tools, and wash them regularly.
- Clean contaminated surfaces: Disinfect areas where fungi may be present, such as shower floors and gym equipment.
3. Wear Appropriate Clothing
Choose loose-fitting, breathable clothing made from natural fibers like cotton. Avoid tight garments and opt for moisture-wicking materials during exercise to keep the skin dry.
4. Protect Your Feet
To prevent tinea pedis, also known as athlete’s foot, take these precautions:
- Wear flip-flops: Use flip-flops or sandals in communal showers and locker rooms.
- Keep feet dry: Change socks regularly and choose moisture-wicking materials. Allow shoes to air out between uses.
5. Manage Underlying Health Conditions
If you have a health condition that predisposes you to infections, work with your healthcare provider to manage it effectively. Keeping conditions like diabetes under control can significantly reduce the risk of recurrent tinea.
6. Monitor and Treat Pets
Regular veterinary check-ups for pets can help detect and treat dermatophyte infections early, preventing transmission to humans. Practice good hygiene when handling pets and their belongings.
7. Boost Immune Health
Supporting your immune system can enhance your body’s ability to fend off infections. Maintain a balanced diet, get regular exercise, manage stress, and ensure adequate sleep.
SEE ALSO: Is Ringworm Considered a Parasite?
Effective Treatment Options
While prevention is key, effective treatment is crucial for eradicating tinea infections. Various treatment options are available, depending on the severity and location of the infection:
1. Topical Antifungals
For mild to moderate infections, topical antifungal creams, lotions, or powders are often effective. Common active ingredients include:
- Clotrimazole
- Miconazole
- Terbinafine
- Ketoconazole
Apply these medications as directed, typically for 2-4 weeks, even if symptoms improve sooner.
2. Oral Antifungals
For more severe or widespread infections, oral antifungal medications may be necessary. These include:
- Terbinafine
- Itraconazole
- Fluconazole
Oral treatments are usually prescribed for several weeks to ensure complete eradication of the infection.
3. Adjunctive Therapies
In addition to antifungal medications, other treatments may help manage symptoms and prevent recurrence:
- Antifungal shampoos: For tinea capitis, medicated shampoos containing selenium sulfide or ketoconazole can reduce fungal spores on the scalp.
- Moisture control: Using powders or sprays to keep areas like the feet and groin dry can prevent fungal growth.
- Skin barrier repair: Moisturizing creams with barrier-enhancing ingredients can help restore the skin’s protective function.
The Role of Healthcare Providers
Healthcare providers play a crucial role in diagnosing and managing tinea infections. They can:
1. Accurately diagnose: Misdiagnosis can lead to inappropriate treatment. Providers can confirm tinea through physical examination and, if necessary, laboratory tests like skin scrapings or fungal cultures.
2. Prescribe appropriate treatment: Based on the type and severity of the infection, providers can recommend the most effective antifungal medications.
3. Educate patients: Guidance on proper treatment application, hygiene practices, and prevention strategies can empower patients to manage their condition effectively.
4. Monitor progress: Follow-up appointments ensure that the infection is responding to treatment and allow for adjustments if needed.
Conclusion
Tinea infections, though common and often manageable, can be a persistent and recurrent problem for many individuals. Understanding the factors that contribute to recurrence, such as incomplete treatment, environmental reinfection, underlying health conditions, personal habits, and genetic susceptibility, is essential for effective prevention and management.
By completing the full course of treatment, maintaining good hygiene, wearing appropriate clothing, managing health conditions, monitoring pets, and supporting immune health, individuals can significantly reduce the risk of recurrent tinea infections. Additionally, seeking professional medical advice and following prescribed treatments diligently are key steps in achieving long-term relief from this frustrating condition.
With a comprehensive approach that combines effective treatment and proactive prevention strategies, it is possible to break the cycle of recurrent tinea infections and maintain healthy, fungus-free skin.
Related Topics: